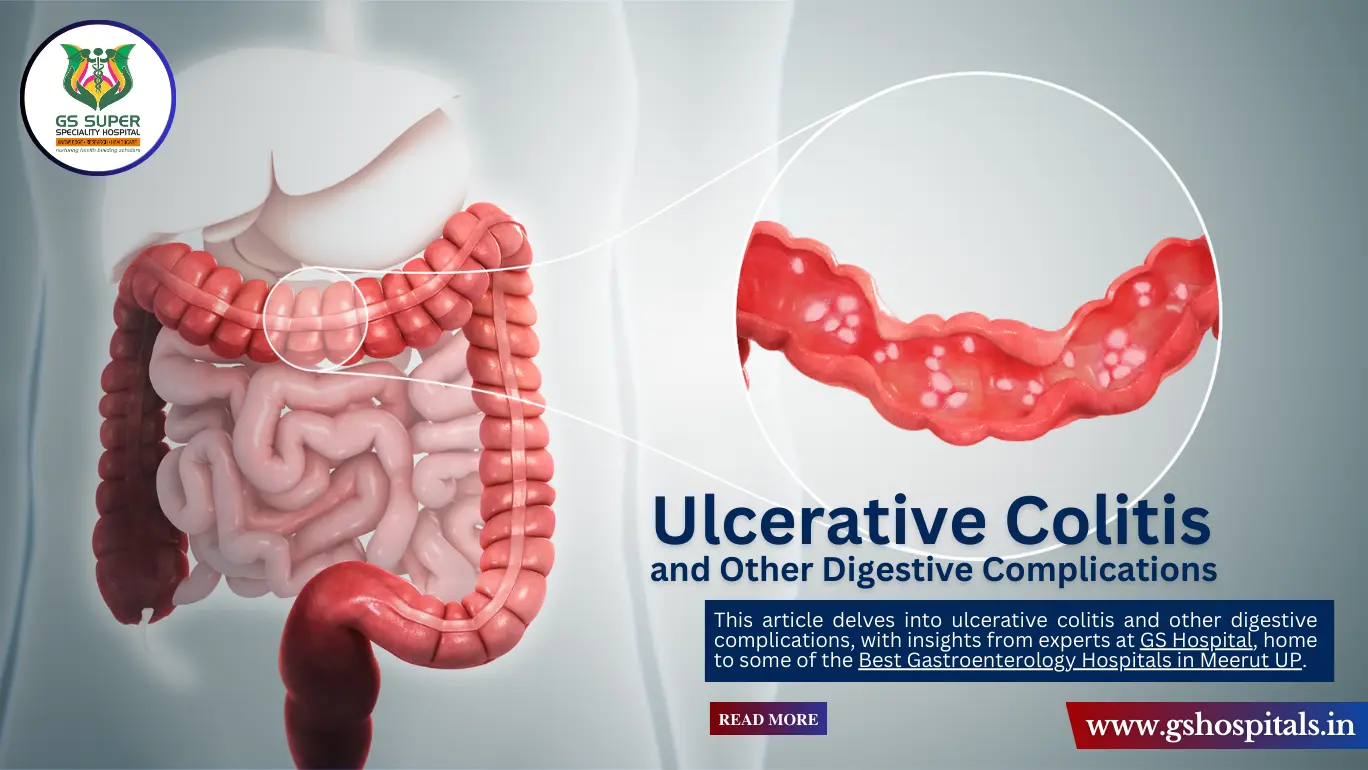
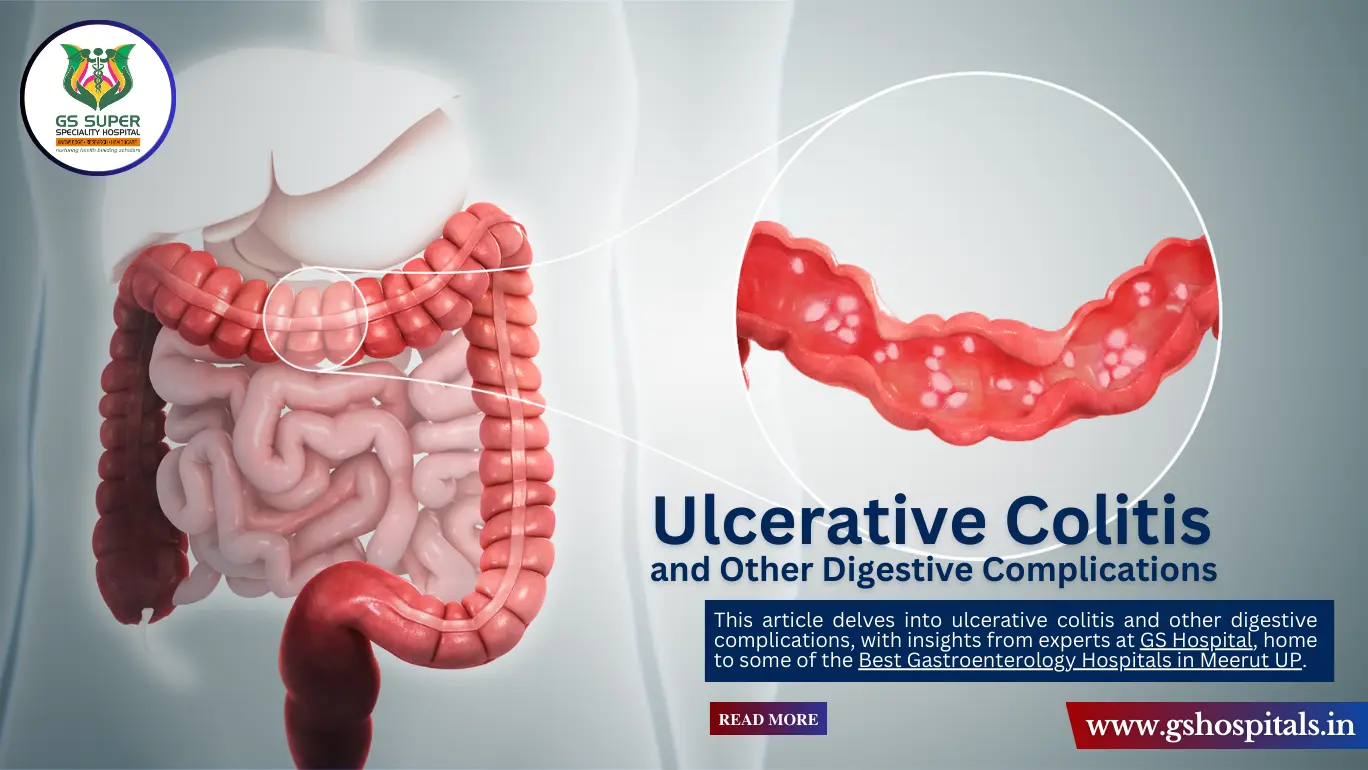
Ulcerative Colitis and Other Digestive Complications
Published On : July 01, 2024
Digestive health plays a critical role in overall well-being. Unfortunately, many people suffer from conditions that disrupt their digestive system, such as ulcerative colitis and other related complications. Understanding these conditions, their symptoms, and available treatments is essential for managing them effectively. This article delves into ulcerative colitis and other digestive complications, with insights from experts at GS Hospital, home to some of the Best Gastroenterology Hospitals in Meerut UP.
Digestive disorders can range from mild discomfort to severe, life-altering conditions. Among these, ulcerative colitis is a significant chronic condition that primarily affects the colon and rectum. Understanding and managing this condition, along with other digestive complications, is essential for maintaining gastrointestinal health.
What is Ulcerative Colitis?
Definition and Overview:
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. It causes inflammation and ulcers (sores) in the lining of the large intestine, leading to various gastrointestinal symptoms. Unlike Crohn's disease, which can affect any part of the gastrointestinal tract, ulcerative colitis is confined to the colon and rectum. This condition can significantly impact a person’s quality of life, necessitating ongoing medical treatment and lifestyle adjustments.
Symptoms of Ulcerative Colitis:
Common symptoms of ulcerative colitis include:
- Persistent Diarrhea: Frequent and urgent bowel movements, often with blood or pus.
- Abdominal Pain and Cramping: Painful episodes in the lower abdomen, often relieved after a bowel movement.
- Rectal Bleeding: The presence of blood in the stool, which can vary from minor streaks to significant amounts.
- Urgency to Defecate: A sudden and intense need to have a bowel movement.
- Weight Loss: Unintended weight loss due to decreased appetite and nutrient malabsorption.
- Fatigue: Persistent tiredness and low energy levels, often due to anemia or the body’s response to chronic inflammation.
- Fever: Low-grade fevers that may occur during flare-ups.
Variability and Flare-Ups:
The severity of symptoms in ulcerative colitis can vary greatly among individuals. Some people may experience mild symptoms, while others have severe and debilitating symptoms. The disease course is often characterized by periods of remission, where symptoms are minimal or absent, interspersed with flare-ups, during which symptoms become more pronounced.
- Periods of Remission: Times when symptoms are minimal or completely absent.
- Flare-Ups: Episodes where symptoms worsen and become more intense, requiring adjustments in treatment.
Impact on Quality of Life:
Ulcerative colitis can significantly affect a person’s daily life, including their ability to work, engage in social activities, and maintain a healthy diet. The unpredictability of flare-ups can cause anxiety and stress, further exacerbating the condition. Therefore, comprehensive management, including medication, lifestyle changes, and psychological support, is crucial for improving the quality of life for those living with ulcerative colitis.
Causes and Risk Factors:
Genetic Factors:
Genetics play a significant role in the development of ulcerative colitis (UC). Individuals with a family history of inflammatory bowel disease (IBD), which includes both ulcerative colitis and Crohn's disease, are at a higher risk of developing the condition. Studies have shown that certain genetic mutations are associated with an increased susceptibility to UC. While genetics alone do not determine whether someone will develop UC, they do contribute to a person’s overall risk.
- Family History: Having a close relative with IBD significantly increases the risk of developing UC.
- Genetic Mutations: Specific genetic mutations have been linked to a higher likelihood of UC.
Immune System Dysfunction:
Ulcerative colitis is believed to involve an abnormal immune response. In a healthy immune system, the body’s defense mechanisms target harmful pathogens. However, in individuals with UC, the immune system mistakenly attacks the cells in the colon, causing chronic inflammation and ulceration. This dysfunction is not entirely understood but is thought to result from a combination of genetic predisposition and environmental factors.
- Autoimmune Response: The immune system erroneously targets the colon’s lining.
- Chronic Inflammation: Ongoing immune attacks lead to persistent inflammation and ulceration.
Environmental Triggers:
Environmental factors can also play a critical role in triggering or exacerbating ulcerative colitis symptoms. These factors are varied and can include lifestyle choices, stress, and external exposures. Understanding and managing these triggers is essential for controlling the disease.
- Diet: Certain foods can exacerbate symptoms. High-fat diets and processed foods are often linked to flare-ups.
- Stress: Emotional and psychological stress can trigger symptom onset or worsen existing symptoms.
- Smoking: While smoking is a known risk factor for Crohn’s disease, it has been observed that former smokers are at a higher risk for developing UC than those who have never smoked.
- Infections: Gastrointestinal infections can trigger UC symptoms or flare-ups.
- Medications: The use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, can worsen symptoms and may trigger the onset of the disease in some individuals.
Diagnosis of Ulcerative Colitis:
Medical History and Physical Examination:
The diagnostic process for ulcerative colitis (UC) starts with a comprehensive medical history and physical examination. During this initial evaluation, patients are asked detailed questions about their symptoms, including the onset, duration, and severity of symptoms like diarrhea, abdominal pain, and rectal bleeding. Physicians also inquire about the patient's family history of inflammatory bowel diseases (IBD) and any other relevant medical conditions. A physical examination may include checking for abdominal tenderness, distension, and signs of malnutrition or anemia.
- Symptom Review: Detailed questions about gastrointestinal symptoms.
- Family History: Inquiry into family history of IBD.
- Physical Exam: Checking for abdominal pain and other physical signs.
Laboratory Tests:
Laboratory tests play a crucial role in the diagnosis of UC. Blood tests are conducted to check for signs of inflammation, anemia, and other abnormalities. Common blood tests include complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Stool samples are also analyzed to rule out infections and other conditions that could cause similar symptoms.
- Blood Tests: CBC, ESR, and CRP to detect inflammation and anemia.
- Stool Samples: Tests to rule out infections and other gastrointestinal conditions.
Endoscopic Procedures:
Endoscopic procedures are essential for directly visualizing the interior of the colon and obtaining tissue samples. The two main procedures used are colonoscopy and sigmoidoscopy. During a colonoscopy, a long, flexible tube with a camera is inserted through the rectum to examine the entire colon. Sigmoidoscopy is similar but focuses on the rectum and lower part of the colon. These procedures allow doctors to identify inflammation, ulcers, and bleeding, and to take biopsies for histological examination.
- Colonoscopy: Examination of the entire colon using a flexible tube with a camera.
- Sigmoidoscopy: Focused examination of the rectum and lower colon.
- Sigmoidoscopy: Focused examination of the rectum and lower colon.
Imaging Studies:
Imaging studies provide additional insights into the condition of the colon and surrounding tissues. X-rays, CT scans, and MRIs are used to detect complications and inflammation that might not be visible through endoscopic procedures alone. These imaging techniques help identify the extent of inflammation, thickening of the intestinal wall, abscesses, and other complications.
- X-Rays: Initial imaging to detect major abnormalities.
- CT Scans: Detailed cross-sectional images of the colon.
- MRIs: High-resolution images to assess the extent of inflammation and other complications.
Treatment Options for Ulcerative Colitis:
Medications:
Several types of medications are used to treat ulcerative colitis, each with a specific role in managing the disease:
- Aminosalicylates: These drugs, such as mesalamine, help reduce inflammation in the lining of the intestine and are often used for mild to moderate cases of ulcerative colitis.
- Corticosteroids: Used for short-term control of flare-ups, corticosteroids like prednisone reduce inflammation rapidly. However, they have significant side effects, including weight gain, osteoporosis, and increased risk of infections.
- Immunomodulators: Drugs such as azathioprine and 6-mercaptopurine suppress the immune system to prevent it from attacking the colon. They are often used for patients who do not respond to aminosalicylates or corticosteroids.
- Biologics: These targeted therapies, including infliximab and adalimumab, block specific proteins involved in inflammation, such as tumor necrosis factor (TNF). Biologics are typically used for moderate to severe cases of ulcerative colitis or when other treatments fail.
Lifestyle and Dietary Changes:
Lifestyle and dietary modifications play a crucial role in managing symptoms and preventing flare-ups in patients with ulcerative colitis. Key recommendations include:
- Balanced Diet: Following a balanced diet rich in nutrients can help maintain overall health and support the immune system.
- Avoid Trigger Foods: Patients should avoid foods that trigger symptoms, such as spicy foods, alcohol, caffeine, and high-fiber foods during flare-ups.
- Stay Hydrated: Adequate hydration is essential, especially during episodes of diarrhea.
- Regular Exercise: Engaging in regular physical activity can improve overall health and reduce stress.
- Stress Management: Techniques such as mindfulness, meditation, and yoga can help manage stress, which can exacerbate symptoms.
Surgical Interventions:
Surgery may be necessary for patients who do not respond to medications or develop severe complications such as severe bleeding, perforation, or cancer. The most common surgical procedure for ulcerative colitis is a proctocolectomy, which involves:
- Proctocolectomy: This surgery involves removing the entire colon and rectum. After this procedure, patients may need an ileostomy, where the small intestine is diverted through an opening in the abdomen, or an ileoanal anastomosis (J-pouch surgery), which creates a new rectum from the end of the small intestine.
- Other Surgical Options: In some cases, less extensive surgeries may be performed to remove only the diseased sections of the colon.
Complications of Ulcerative Colitis:
Ulcerative colitis, a chronic inflammatory bowel disease, can lead to several serious complications if not managed properly. Understanding these potential issues is crucial for timely intervention and treatment.
Colon Cancer:
- Increased Risk: Patients with long-standing ulcerative colitis have a significantly higher risk of developing colon cancer. This risk increases with the duration and extent of the disease, particularly if the entire colon is affected.
- Screening and Surveillance: Regular screening and surveillance through colonoscopy are essential for early detection and prevention of colon cancer. During these screenings, biopsies may be taken to identify any precancerous changes.
Severe Bleeding:
- Ulcers: Severe bleeding can occur from ulcers in the colon, which are sores caused by ongoing inflammation.
- Blood Loss and Anemia: Significant blood loss from these ulcers can lead to anemia, characterized by fatigue, weakness, and shortness of breath. Severe cases may require blood transfusions or surgical intervention.
Perforated Colon:
- Life-Threatening: A perforated colon, or a hole in the colon, is a life-threatening complication. It can result in the leakage of intestinal contents into the abdominal cavity, leading to peritonitis, a severe abdominal infection.
- Immediate Medical Attention: This condition requires immediate medical attention and often surgical repair to prevent fatal outcomes.
Toxic Megacolon:
- Severe Complication: Toxic megacolon is a rare but severe complication where the colon rapidly expands and becomes paralyzed. This can lead to a buildup of gas and feces, causing the colon to swell.
- Risk of Rupture: If untreated, toxic megacolon can cause the colon to rupture, leading to life-threatening infections and sepsis.
- Emergency Treatment: Treatment typically involves medications to reduce inflammation and bowel rest. In severe cases, emergency surgery to remove the affected portion of the colon may be necessary.
Additional Complications:
- Primary Sclerosing Cholangitis: This is a liver disease that causes scarring and inflammation of the bile ducts, often associated with ulcerative colitis.
- Bone Loss: Chronic inflammation and steroid use can lead to osteoporosis, increasing the risk of fractures.
- Nutritional Deficiencies: Malabsorption of nutrients due to chronic diarrhea can result in deficiencies in vitamins and minerals, necessitating dietary adjustments or supplements.
Other Digestive Complications:
Crohn's Disease - Overview and Symptoms:
- Definition: Crohn's disease is another form of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from the mouth to the anus.
- Symptoms: Common symptoms include chronic diarrhea, abdominal pain, weight loss, fatigue, and malnutrition. The inflammation caused by Crohn's disease can spread deep into the layers of affected bowel tissue, leading to debilitating symptoms and complications such as strictures and fistulas.
Treatment Options:
- Medications: Treatment typically involves anti-inflammatory drugs, immune system suppressors, antibiotics, biologics, and symptomatic relief medications like antidiarrheals.
- Lifestyle Changes: Dietary adjustments, such as eating smaller, more frequent meals and avoiding certain trigger foods, can help manage symptoms.
- Surgery: Surgery may be necessary to remove damaged portions of the digestive tract, manage complications, or relieve symptoms when other treatments are ineffective.
Irritable Bowel Syndrome (IBS):
Overview and Symptoms:
- Definition: Irritable bowel syndrome (IBS) is a functional digestive disorder characterized by chronic abdominal pain, bloating, and changes in bowel habits, such as diarrhea, constipation, or alternating between both.
- Non-Inflammatory: Unlike IBD, IBS does not cause inflammation or permanent damage to the intestines. It is believed to be related to abnormalities in gut-brain interaction, motility issues, and increased sensitivity of the intestines.
Treatment Options:
- Dietary Changes: Following a low-FODMAP diet, increasing fiber intake, and avoiding foods that trigger symptoms can help manage IBS.
- Medications: Treatment may include antispasmodics, laxatives, anti-diarrheal agents, and medications to manage pain and discomfort.
- Stress Management: Techniques such as cognitive-behavioral therapy (CBT), relaxation exercises, and regular physical activity can help reduce stress, which often exacerbates IBS symptoms.
Celiac Disease:
Overview and Symptoms:
- Definition: Celiac disease is an autoimmune disorder in which ingestion of gluten a protein found in wheat, barley, and rye triggers an immune response that damages the small intestine.
- Symptoms: Symptoms include chronic diarrhea, bloating, abdominal pain, weight loss, and malnutrition. Non-digestive symptoms can also occur, such as anemia, osteoporosis, skin rashes, and neurological issues.
Treatment Options:
- Gluten-Free Diet: The primary treatment for celiac disease is a strict gluten-free diet, which helps heal the intestine and prevents further damage and symptoms. Patients must avoid all foods and products containing gluten.
- Nutritional Support: Due to potential malabsorption, patients may need supplements to correct deficiencies in vitamins and minerals such as iron, calcium, vitamin D, and B vitamins.
- Regular Monitoring: Follow-up care includes regular medical check-ups and blood tests to monitor for complications and ensure adherence to the gluten-free diet.
The Role of Gastroenterologists:
Expertise in Diagnosis and Treatment:
Gastroenterologists specialize in diagnosing and treating digestive disorders. At GS Hospital, some of the best gastroenterologists in Ghaziabad and UP provide expert care for patients with conditions like ulcerative colitis, Crohn's disease, IBS, and celiac disease.
Importance of Regular Check-Ups:
Regular check-ups with a gastroenterologist are crucial for managing chronic digestive conditions. These appointments allow for monitoring disease progression, adjusting treatment plans, and addressing any new symptoms or complications.
Advances in Gastroenterology:
Research and Innovations:
Continuous research and innovations in gastroenterology are improving the diagnosis and treatment of digestive disorders. Advances in endoscopic techniques, biologic therapies, and personalized medicine are enhancing patient outcomes.
Telemedicine and Remote Monitoring:
Telemedicine and remote monitoring technologies are making it easier for patients to access care and manage their conditions from the comfort of their homes. These technologies provide convenience and improve adherence to treatment plans.
Living with Ulcerative Colitis and Other Digestive Conditions:
Coping Strategies:
Living with a chronic digestive condition requires effective coping strategies. Patients can benefit from:
- Support Groups: Joining support groups provides emotional support and valuable insights from others who understand their experiences.
- Stress Management: Techniques like meditation, yoga, and counseling can help manage stress, which can exacerbate symptoms.
- Staying Informed: Keeping up with the latest information about their condition empowers patients to make informed decisions about their care.
Conclusion
Ulcerative colitis and other digestive complications present significant challenges, but with the right care and management, patients can achieve better health outcomes. GS Hospital, known for having some of the Best Gastroenterologists in UP, offers comprehensive care for these conditions. By staying informed, seeking regular medical care, and adopting healthy lifestyle habits, patients can effectively manage their digestive health.
FAQs
1. What are the common symptoms of ulcerative colitis?
Common symptoms of ulcerative colitis include persistent diarrhea, abdominal pain, rectal bleeding, urgency to defecate, weight loss, fatigue, and fever.
2. How is ulcerative colitis diagnosed?
Ulcerative colitis is diagnosed through a combination of medical history, physical examination, laboratory tests, endoscopic procedures, and imaging studies.
3. What treatment options are available for ulcerative colitis?
Treatment options for ulcerative colitis include medications (such as aminosalicylates, corticosteroids, immunomodulators, and biologics), lifestyle and dietary changes, and surgical interventions.
4. How can I manage my ulcerative colitis symptoms?
Managing ulcerative colitis symptoms involves following a balanced diet, avoiding trigger foods, staying hydrated, exercising regularly, managing stress, and adhering to prescribed medications.
5. What role do gastroenterologists play in treating digestive disorders?
Gastroenterologists specialize in diagnosing and treating digestive disorders. They provide expert care, monitor disease progression, adjust treatment plans, and address complications, helping patients manage their conditions effectively.
6. What other digestive complications does GS Hospital treat?
Best Gastrologist in Ghaziabad, GS Hospital treats a range of digestive complications, including Crohn’s disease, IBS, GERD, and celiac disease, among others.